Many people understand the short-term effects of alcohol—like a buzzed feeling or temporary relaxation. But far fewer realize the long-term consequences, especially when it comes to mental health. Alcohol misuse doesn’t just impact your body—it can significantly worsen conditions like clinical depression and anxiety.
Let’s explore how alcohol and depression are connected, why alcohol is not a healthy coping mechanism, and how to seek help if you or a loved one is struggling.
🧠 Depression and Alcohol: A Dangerous Mix
Clinical depression is a serious mood disorder that affects how a person thinks, feels, and functions. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), major depressive disorder (MDD) is diagnosed when a person experiences at least two weeks of persistent sadness or low mood, plus additional symptoms such as:
-
Loss of interest or pleasure in activities
-
Fatigue or low energy
-
Sleep disturbances (insomnia or hypersomnia)
-
Changes in appetite or weight
-
Feelings of worthlessness or guilt
-
Trouble concentrating or making decisions
-
Thoughts of death or suicide
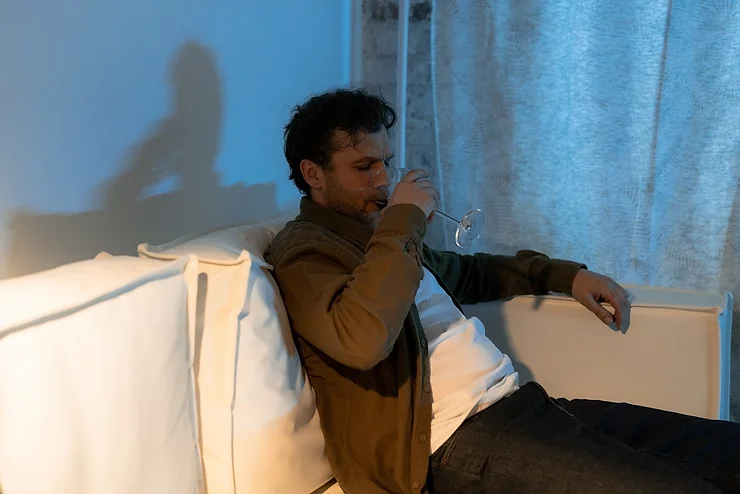
In an attempt to manage these overwhelming symptoms, some people turn to alcohol as a form of self-medication. Unfortunately, this only compounds the problem.
🍷 Why Alcohol Makes Depression Worse
At first, alcohol may seem to help. It can produce short-term feelings of euphoria, lower social inhibitions, and temporarily dull feelings of sadness or anxiety. But alcohol is a central nervous system depressant—which means it slows brain function and affects mood-regulating chemicals like serotonin and dopamine.
Here’s what really happens:
-
Temporary relief is followed by a crash: After that initial “feel-good” phase, alcohol can lead to increased sadness, irritability, and fatigue.
-
Disrupted brain chemistry: Regular alcohol use throws off the balance of neurotransmitters that regulate mood.
-
Worsening symptoms: Depression may deepen as alcohol increases feelings of hopelessness, confusion, or emotional instability.
-
Physical withdrawal: As your body becomes dependent, withdrawal can increase anxiety, insomnia, and agitation, creating a vicious cycle.
🔁 The Cycle of Self-Medication
People with depression who drink to numb emotional pain may find themselves trapped in a cycle of alcohol dependence. This often leads to:
-
Increased frequency and quantity of drinking
-
Heightened symptoms of both depression and anxiety
-
Trouble functioning at work, in relationships, and in daily life
-
Suicidal thoughts or behaviors
According to mental health professionals, co-occurring disorders—such as depression and alcohol use disorder (AUD)—are common and often stem from shared risk factors like:
-
A family history of depression or addiction
-
Past trauma or abuse
-
Chronic stress or environmental hardship
-
Untreated mental health conditions
⚠️ The Physical Effects of Alcohol on the Body
Beyond mental health concerns, long-term alcohol use can cause serious damage to your physical health:
💧 Dehydration
Alcohol is a diuretic—it increases urination and can cause dehydration, leading to fatigue, dizziness, and headaches.
🫀 Liver Damage
Your liver metabolizes alcohol, and excessive drinking over time can cause inflammation, fatty liver, or even cirrhosis.
❤️ Heart Disease
Heavy drinking increases the risk of high blood pressure, heart attack, and irregular heartbeat.
🎗️ Cancer
Alcohol is a known carcinogen and has been linked to various cancers, including breast, liver, esophageal, and colorectal cancers.
🛑 Why You Shouldn’t Use Alcohol to Cope with Depression
Using alcohol to self-soothe may feel like a quick fix—but it’s a band-aid on a much deeper issue. If you rely on alcohol to handle depression or anxiety, you’re likely delaying the real healing that comes from therapy, lifestyle changes, and professional support.
💬 What to Do If You or a Loved One Is Struggling
If you suspect that alcohol is affecting your mental health—or someone you love is using alcohol to cope—don’t ignore it. You’re not alone, and there are effective treatment options available.
✅ Steps You Can Take:
-
Talk to a licensed mental health professional
-
Look into dual diagnosis treatment for co-occurring disorders
-
Connect with support groups, such as AA or SMART Recovery
-
Discuss concerns with your doctor if you’re unsure how to start
Recovery is possible. With the right support, you can learn healthier coping strategies, treat both depression and alcohol misuse, and improve your quality of life.
🧩 Final Thoughts
The relationship between alcohol and depression is complex—but clear: alcohol doesn’t cure depression—it worsens it. Recognizing this connection is the first step toward healing. If you’re concerned about your alcohol use and mental health, reach out. Support is available, and you deserve to feel better.